Heart blocks develop silently, but they can come on suddenly. While medical tests remain the gold standard for diagnosis, learning how to manage heart block at home with symptoms and essential monitoring could save your life.
This guide details warning signs, practical home checks, and when to seek immediate medical attention.
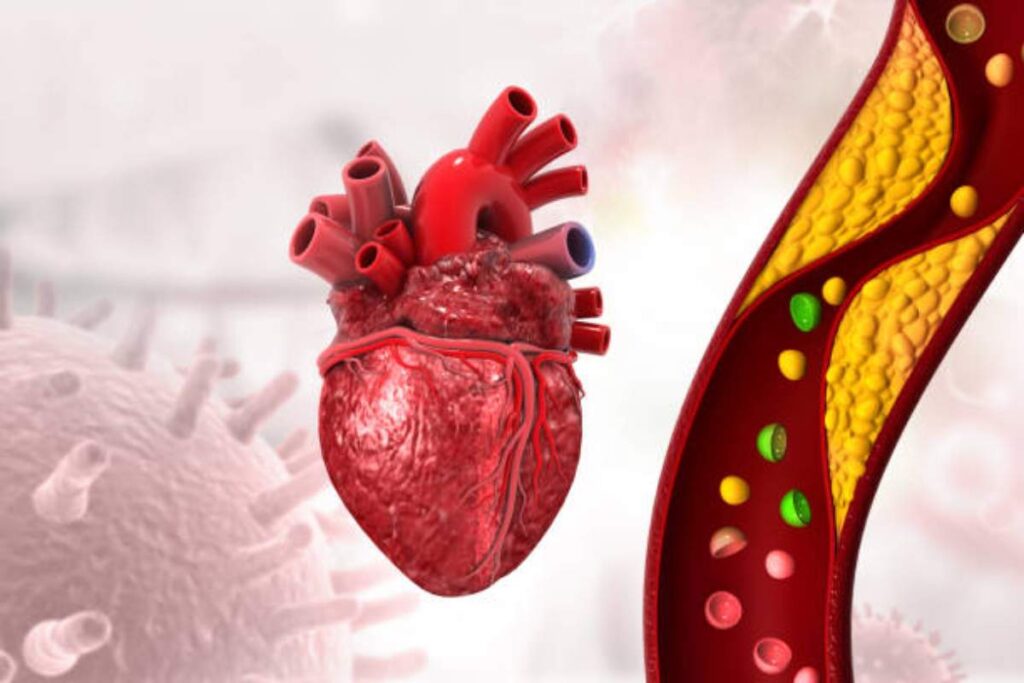
What Is a Heart Blockage?
Heart block occurs when plaque (fat, cholesterol, and calcium) builds up in the coronary arteries. Over time, this restricts blood flow and deprives the heart of oxygen.
Partial blockages may not cause symptoms at first, but severe cases cause chest pain, heart attack, or sudden collapse.
Key symptoms to watch for at home
- Recognizing the early symptoms is the first step in managing heart block at home. Look for:
- Chest discomfort: Pressure, tightness, or burning that worsens with activity.
- Shortness of breath: Difficulty breathing after light tasks such as climbing stairs.
- Unexplained fatigue: Feeling exhausted despite adequate rest.
- Dizziness or nausea: Episodes related to exertion or stress.
Symptoms by degree:
- Mild: Pain only during intense exercise.
- Moderate: Discomfort when walking briskly or in cold weather.
- Severe: Symptoms are present when walking slowly or at rest.
- Note: Chest pain that radiates to the jaw, back, or arms requires immediate attention.
Can You Test for Heart Blockage Without a Doctor?
No. Home methods only indicate problems but cannot confirm blockages. However, monitoring these indicators can help spot red flags:
| Home Check | How to Do It | What It Tells You |
| Blood Pressure Monitor | Sit calmly for 5 minutes, then use a digital BP monitor on your upper arm. | High readings signal artery stress. |
| Pulse Rate | Check the pulse of your wrist or neck for 60 seconds; use a heart rate monitor if available. | Irregular rhythms or high resting rates may indicate heart issues. |
| Stair Test | Time yourself climbing 60 stairs (or 30 up and down) within 90 seconds. | Fatigue or breathlessness can signal heart or lung problems. |
| Symptom Journal | Record chest pain occurrences, noting time, duration, and triggers. | Tracking pain helps identify patterns and potential heart concerns. |
Example: If your blood pressure is higher than 140/90 mmHg or you can’t do the stair test without gasping, contact your doctor.
How to monitor your heart health every day
- Monitor your blood pressure: Use an FDA-approved cuff. Check twice a day while seated. Ideal: less than 120/80 mmHg.
- Measure your resting heart rate: Place two fingers on your wrist. Count the beats for 60 seconds. Standard: 60–100 ppm.
- Log symptoms: Note any chest tightness, shortness of breath, or dizziness with time stamps.
Pro tip: Sync your data with apps like Apple Health or Google Fit to see trends.
When Home Checks Aren’t Enough?
While learning how to manage heart block at home is helpful, some signs require a trip to the emergency room:
- Crushing chest pain that lasts more than 15 minutes: If the pain persists for a long time and doesn’t go away, it could mean your heart is suffering from heart block.
- Cold sweats with vomiting: Clammy skin and discomfort can indicate your heart is stressed.
- Fainting or inability to stand: Weak legs and blurred vision can indicate that your heart lacks blood flow.
- Sharp pain in your arm or jaw: Pain moving to your left side or jaw can indicate your heart is under stress.
- Rapid breathing without cause: An overworked heart may need help quickly.
- Chest tightness that gets worse over time: If your chest feels like a rock and won’t go away, get help.
- Heart beats too fast or too slow: A heart that is out of sync can put you at risk for further damage.
- Weak but cold hands and feet: The heart may not work correctly if blood doesn’t reach all parts.
Remember: Delaying care during a heart attack increases damage to the heart muscle.
What doctors use to diagnose blockages
- If home monitoring is a concern, doctors may order:
- Electrocardiogram (ECG): Checks for irregular heart rhythms.
- Stress test: Measures how well the heart performs during exercise.
- Coronary angiogram: An X-ray video showing blocked arteries.
- Blood tests: Check cholesterol, triglycerides, and markers of inflammation.
- Echocardiogram: Uses soundscreens to create images of the heart.
- Cardiac CT scan: Special X-ray tests that show details of the heart.
- Cardiac MRI: Provides full pictures of the heart.
- Holter monitoring: Check your heart rhythm for 24 hours or more.
Prevent and reverse early accidents.
- Eat Mediterranean style: Focus on fish, olive oil, nuts, and vegetables. A meal rich in healthy fats helps keep blood vessels clear.
- Exercise daily: Take a brisk 30-minute walk. Move every day to keep blood vessels wide and clear.
- Quit smoking: Nicotine increases plaque growth. Quit smoking to prevent plaque from blocking your airways.
- Manage stress: Yoga or deep breathing reduces cortisol. A calm mind allows the heart to function smoothly and lightly.
- Get plenty of sleep: At least 7 hours a night. A rested heart stays strong and beats easily.
- Drink more water: Stay hydrated. Water keeps blood flowing and moving quickly.
- Limit salt: Avoid foods high in sodium. Less salt means less stress on your heart.
- Cut back on sugar: Avoid soda and sweets. Sugar turns into fat, which clogs the blood vessels in your heart.
Take action before it’s too late.
Learning to manage heart block at home will help you detect risks early. However, never self-diagnose. Use home monitoring as a guide, not a substitute for medical care. See a cardiologist right away if symptoms persist. Share this guide with your family—it could save a life.
Think you have heart block? Don’t wait. Schedule a consultation with a cardiology specialist today. Click here to find a cardiologist near you.
Frequently Asked Questions
Can stress cause heart blockages?
Yes. Chronic stress increases blood pressure and inflammation, accelerating plaque buildup.
Does family history affect my risk?
Absolutely. Genetic factors influence cholesterol levels and artery health.
Are blocks reversible?
Early plaque can be reduced with diet, exercise, and medications such as statins.
How often should I monitor my blood pressure at home?
If you are over 40 or at high risk, check weekly. Others: monthly.
What foods prevent blockages?
Oats, berries, oily fish, and garlic lower LDL cholesterol.
Is chest pain always a heart problem?
No. Acid reflux or muscle tension can mimic it. But keep it under control.
Can young adults get heart block?
Yes. Obesity, vaping, and poor diet increase rates of blockage in those under 40.